Agile Engagement and Behavior Change
Health plans often struggle with slow, outdated communication processes, siloed technology systems, and inconsistent member outreach. These inefficiencies lead to increased operational costs, missed opportunities to engage members effectively, and ultimately, poor health outcomes.
Moreover, many plans face the challenge of implementing behavioral change strategies that drive engagement and improve member health, while also managing the complexity of personalization across multiple channels.
Engagys has pioneered a solution to meet these demands—Agile Engagement and Behavior Change.
Our approach empowers health plans to streamline operations, optimize communications, and deliver personalized member experiences at scale.
Health plans need a scalable, efficient solution to meet these demands—and that’s where Engagys steps in.
Engagys has implemented agile engagement and behavior change at top national health plans driving millions in medical cost and operational savings.
The Agile Engagement Approach
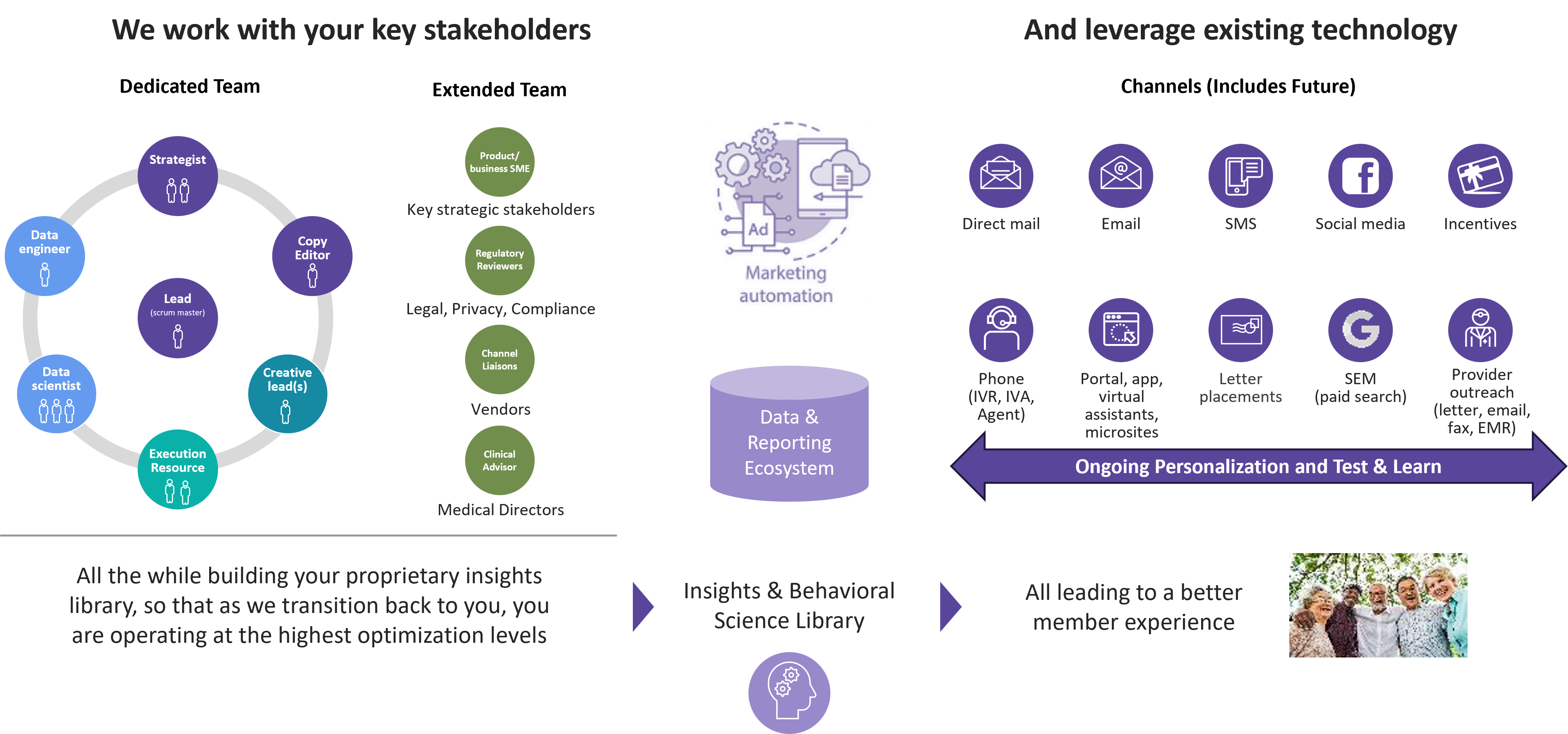
Engagys’ Agile Engagement and Behavior Change approach is purpose-built to help health plans improve member communication and optimize engagement. Here’s how we deliver results:
Rapid Assessment of Capabilities
We begin with a quick assessment of your resources, engagement strategies, data, execution practices, results, and related technologies. This allows us to create a roadmap for operationalizing agile teams and leveraging your existing capabilities for immediate impact.
Agile Team Formation
We set up small engagement teams focused on your priority focus areas to start such as enrollment, onboarding, gaps in care, treatment decision support, behavioral health and/or pharmacy engagement.
These teams operate using rapid 2-3 week sprints, enabling constant iteration and optimization of communication strategies. We provide staffing to fill in the gaps and act as part of the agile teams in the interim until clients are ready to take over operations and implementation.
Behavioral Science Integration
Our approach integrates behavioral science principles— such as framing, incentives, and authority—into member communications. These communication techniques ensure that messages resonate with members, influencing behavior change and improving health outcomes.
Personalizaton at Scale
Our agile approach leverages data and real-time feedback to deliver highly personalized communications across channels. This test-and learn methodology reduces member abrasion and ensures that health plans can maintain relevance in every interaction, all while scaling effectively.
Continuous Improvement
Our solution enables health plans to constantly refine their engagement strategies through ongoing testing and optimization.
We help you stand up and adapt agile engagement processes and teams, working alongside you to scale and optimize, and ultimately transitioning operations to your team. Agile teams can be rolled out over time, allowing organizations to gradually scale while ensuring long-term success.
Real Results
The client: Large, national health plan offering health insurance and similar services such as, dental, vision, pharmacy, Medicare, and Medicaid to meet the needs of individuals, families, employers, and healthcare providers.
The challenge: Client sought to build and scale multiple engagement teams, ensuring cross-departmental collaboration including successful communication experimentation and ongoing optimization.
The solution: Teams created to execute numerous test-and-learn experiments in member communications for commercial and Medicare members to drive behavior change. Defined, implemented, optimized and operated client’s multi-channel agile engagement model leveraging Salesforce.

Get Started with Agile Engagement Today
Ready to accelerate your member engagement strategy with an agile engagement approach? Schedule a meeting with Engagys today to learn how we can help you optimize your communications, improve member experience, and drive cost savings. Together, we can transform how you engage with your members.


