Strategies for Boosting Medicare Advantage Member Retention and Satisfaction

This past fall, health plan payers saw the highest number of Medicare Advantage (MA) members switching plans in seven years during AEP (16% switching) and OEP (7% switching). While cost-cutting efforts are at the top of MA plans’ agendas, members are feeling the squeeze and looking for alternatives that meet their needs.
With continued pressure to reduce spend through administrative cuts and trimmed-down supplemental benefits, payers need to protect their existing membership from the impact. To increase retention, now is the time to not only showcase the benefits a member has, but ensure members understand and engage with their plan effectively.
How to Reduce Member Switching
Engagys understands the key strategies to reduce churn and maintain satisfaction. Our proven techniques to boost member retention include:
Use Data to Get Ahead: Prepare now so you’re not left behind. Payers that are proactive in addressing those members most apt to switch will win in 2025. Clarity, plain language, setting expectations, demonstrating value, and building loyalty early will all be critical drivers of attracting and retaining members.
Enhance the ANOC: Payers must clearly explain benefit changes using compelling educational materials alongside the standard ANOC. Proactively right sizing a member after a negatively-perceived ANOC can significantly boost a plan’s enrollment. For example, Engagys helped one national client achieve a more than 40% higher re-enrollment (compared to a control group) among members at risk of churn due to cost increases, generating millions of incremental revenue.
Level-up During AEP: Payers must uplevel their acquisition marketing for today’s savvy healthcare consumers. Shoppers span channels and priorities, and payer outreach must reflect that. Check your SEO to be sure it’s performing. Communicate across all channels and be sure your social media presence reflects your organization’s mission.
Showcase Supplemental Benefits: Help members use their plans effectively and leave nothing on the table by sending timely reminders encouraging them to exhaust unused benefits—such as a quarterly OTC allowance. These proactive reminders will become mandatory next year with the 2025 Final Rule announcement.
Proactively Enter OEP: Maximize this year’s OEP by proactively communicating with your members to combat your competitors’ reach. Attract your competition’s switchers early—don’t miss an opportunity.
Prepare Call Center Agents Now: Train agents to address common inquiries, react to member concerns related to changes, be prepared to rightsize when needed, and show needed empathy.
Real Results
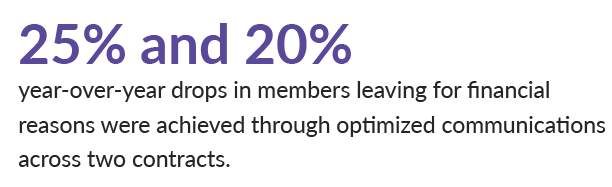
Client: A regional Medicare Advantage plan.
Opportunity: As a premium cost plan, OEP churn was common.
Solution and Results: Engagys helped the plan target, segment populations, and re-position their member messaging during OEP.
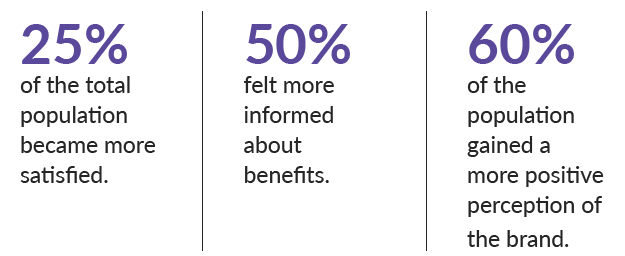
Client: A national health plan serving millions of medical, dental, and pharmacy members.
Opportunity: Members needed help understanding and using their benefits effectively.
Solution and Results: Engagys helped the plan launch a streamlined digital experience to improve the members’ understanding of their health plan.