Medicare Advantage Stars Scores Dropped – What’s Next for Health Plans?

It’s no secret that this year’s Medicare Advantage Stars ratings revealed tough realities for many plans. As the dust settles, executives across the industry are asking, “What’s next?” The competition has ramped up, and with many guardrails implemented during the COVID-19 pandemic now removed, health plans are facing a more challenging environment than ever before.
So, how can you ensure that your plan not only survives but thrives in this new landscape? Keep reading for tips on regaining your competitive edge with enhanced scores.
A Staggering Drop in Scores
This year’s Stars ratings confirmed the suspicions of many: competition among Medicare Advantage Prescription Drug (MAPD) plans has intensified. Fifty-eight contracts fell from 4+ Stars to below 4 stars, covering 6.6 million members. Assuming an average bonus of $400 per member, that’s a staggering $2.6 billion in lost bonuses for plans--funds desperately needed to deliver services.
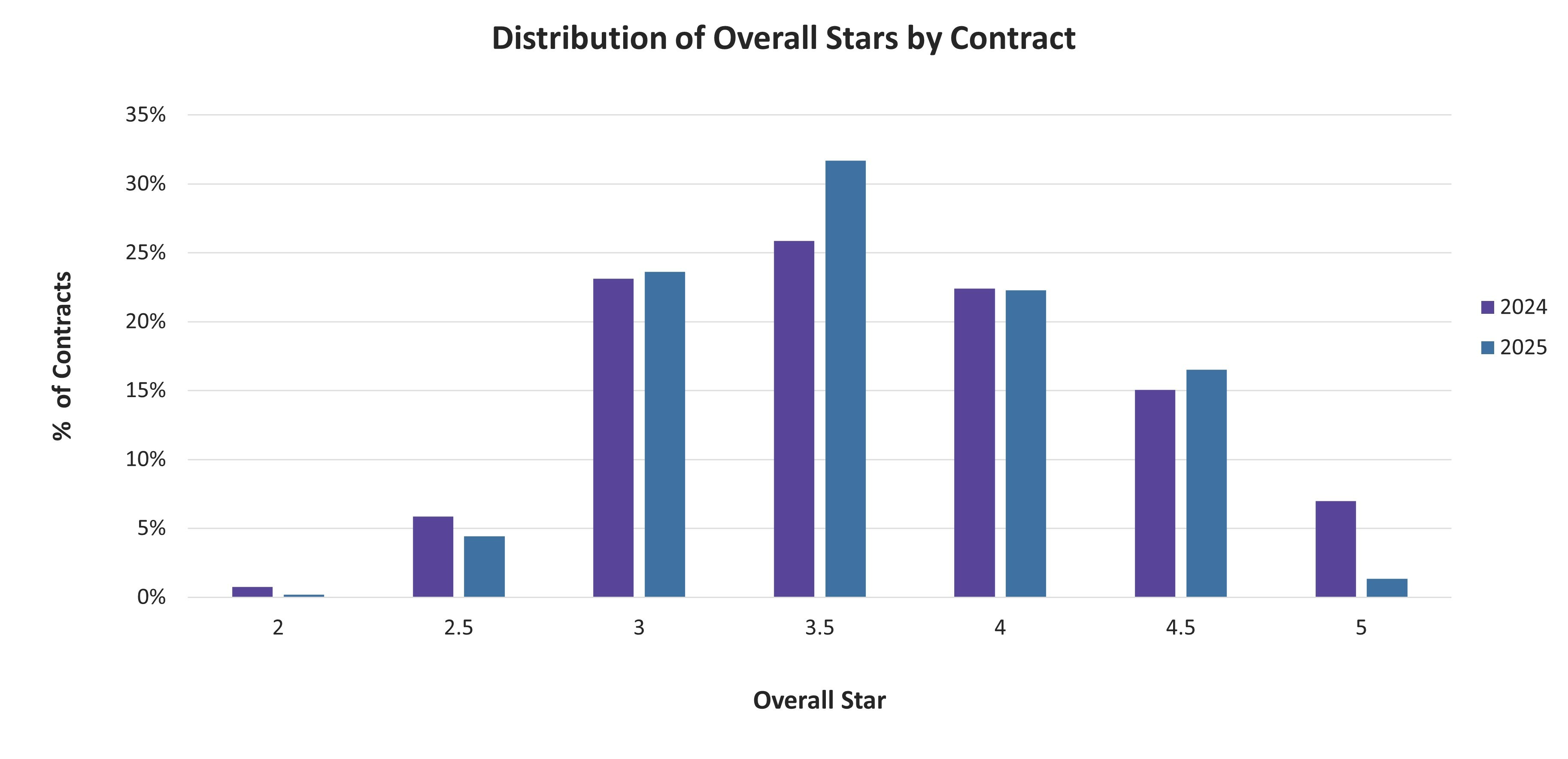
Only seven contracts held on to their 5-Star rating this year. As the chart below demonstrates there was a clear regression toward the mean, with nearly a third of plans now sitting at 3.5-Stars. The bar has been raised, particularly for quality-of-care measures, and plans are feeling the pressure.
Figure 1: Distribution of Overall Stars by Contract
The Challenges of Achieving 4+ Stars
The increasingly competitive nature of Stars can be seen in the changes to the 4-Star cut-points. Achieving 4-Stars was harder for several groups of measures, particularly those related to quality of care.
Table 1: Increases in 4-Star Cut-Points Across Groups of Measures
| +4.3% | Gaps-in-care measures including breast cancer screening, colorectal cancer screening, flu shots, osteoporosis management, eye exams, blood pressure control, and blood sugar control |
| +2.0% | Medication reconciliation, readmissions, transitions of care, follow-up post discharge, statins for members with cardiovascular disease, and statins for members with diabetes |
| +1.9% | CAHPS measures related to member experience |
| +1.7% | HOS measures including falls, bladder control, and monitoring physical activity |
| +1.1% | Adherence measures, such as statins, antihypertensives, and anti-diabetes medications. |
These changes underscore the higher standards set by CMS and the growing competitiveness in the industry. Plans now face a higher bar, and to stay on top, they need to be laser-focused on the areas that will drive the biggest improvements.
How to Regain Your Competitive Edge
Now that it’s Monday morning, what can plans actually do to compete for higher scores in the tougher environment?
The devil is always in the details, but the main idea is to look for groupings and “follow the points.” Whenever we work with clients on Stars scores, we identify the most practical and best “bang for the buck” investments - and develop and implement new processes that can address more than one measure. In context of the table above, there are specific measures that can be addressed by upgrading similar processes and tactics.
1. Adherence: Adherence remains one of the most impactful areas, representing triple-weighted measures that account for 9 points in total, indicating that plans need to double down on adherence efforts. There is a lot of correlation across the three measures (ranging from 0.72 – 0.85). The tactics and analysis needed to improve statins is similar to that needed to drive antihypertensives or anti-diabetes.
Most of our clients recognize that they really need to be proactive and focus on adherence. This time of year, just like in the presidential campaigns, it comes down to doing everything that you can to reach the members who can still help tip the scale. In our work, we have seen this take the form of pharmacist calls, email reminders, and personalized SMS text nudges to get fills and ensure they reach the 80% PDC mark.
But the work doesn’t stop there. In less than three months, the scores will be wiped clean as always, and it will be time to start again. Proven tactics for Q1, like helping members enroll in mail order and educating them on the importance of adherence, are important parts of any onboarding or "welcome back" campaigns.
2. Member experience: The CAHPS measures, while no longer quadruple-weighted, still pack a punch. With 12 points at stake, the member experience remains a key area for plans to focus on. Dig into your mock CAHPS data and look for opportunities. For example, in our work with one client, we found strong correlations between specific questions related to finding information about co-pays and overall plan rating. The inference was that members try to understand their benefits, but hate being surprised. Another client had real challenges with out-of-network utilization and the CAHPS measures related to getting care. The solution was to help members find in-network providers. Solving these pain points—whether it’s simplifying benefit communication or improving network navigation—can significantly boost your scores.
Furthermore, like those for the adherence measures, the cut-points are narrow. Only 4 points separate a 3-Star contract for “Getting Needed Care” from a 5-Star plan. That means any gain can be material.
3. Diabetes care: Diabetes-related measures, including blood sugar and blood pressure control, are another high-impact area. Blood sugar control and blood pressure control are both triple-weighted measures, together with adherence for diabetes medications, use of statins for members with diabetes, and eye exams, there are 9 points specifically tied to this one group.
Creating and executing a holistic approach to care for members with diabetes ought to be a priority. Care managers and additional help desk support can be part of this. Many of our clients are focused on leveraging care management or concierge representatives to help members get the care they need. According to KFF President and CEO Drew Altman, “People report an obstacle course of claims denials, limited in-network providers, and a labyrinth of red tape, with many saying it prevented them from getting needed care.” If plans can remove these obstacles, members will reward them with higher ratings—help them and they will help you.
The Path to 4 Stars and Beyond
While the work to reach four Stars is getting harder, the rewards remain, and it’s not too late to make a difference now - particularly in adherence measures. Now is the time to implement a full-court press, targeting members with gaps in care and preparing robust “welcome back” and onboarding campaigns to tackle member experience measures and CAHPS scores. With the right focus and tactical execution, your health plan can weather the storm and emerge stronger in this increasingly competitive environment. Yes, the path forward is tough, but the rewards for reaching 4 stars are too significant to ignore.
Ready to Improve your Stars Scores?
Engagys specializes in transforming CAHPS, HEDIS, and HOS measures for health plans, resulting in increased member satisfaction and improved health outcomes.
Contact us today to learn how we can help you boost your Stars ratings and maximize your member engagement.


