Segmentation in the New World of AI: A New Frontier for Health Plans

Health plans aim to make every member interaction feel personalized and tailored to their unique journey. A key way they’ve achieved this is by segmenting messaging and communications based on member data and profiles. However, with vast amounts of member data, executing this strategy effectively can be challenging.
With the recent surge of AI-driven technologies in healthcare, health plans have a powerful opportunity to enhance and innovate segmentation efforts. By leveraging data, AI enables health plans to deliver interactions that truly resonate with each member’s unique needs.
Despite the clear opportunities, recent data shows that many health plans are still in the early stages of adopting AI. With decades of experience in member segmentation in parallel with deep expertise on AI enablement for plans, Engagys has key insight into leveraging AI to create targeted, impactful messaging that drives member engagement.
How AI is Shaping Segmentation
As consumers, we're accustomed to hyper-personalized experiences from companies like Amazon or Starbucks, where interactions feel uniquely tailored. This expectation is increasingly spilling over into healthcare, where healthcare consumers seek the same level of relevance and customization in their health interactions. Traditional segmentation has long helped health plans group members based on demographics or common health needs. However, AI takes segmentation beyond demographic boundaries, enabling data-rich, behavior-driven insights that pinpoint the Next Best Action (NBA) for each individual member, known as an N of 1 approach.
For health plans, this means AI can dissect vast amounts of data—claims, engagement records, social determinants, and more—to offer actionable, real-time insights. With AI, segmentation is no longer static. It’s a dynamic, ongoing process that adapts as a member’s circumstances and behaviors change, helping health plans stay relevant in real-time.

Building Effective Segmentation: Start with Behavioral Data
Based on our decades of optimizing healthcare consumer messaging, we’ve learned that behavioral data (over demographic or attitudinal data) is critical. Behavioral data—what members actually do—can be up to five times more predictive of future actions than demographic data alone. In healthcare, this means looking at patterns in health service utilization, medication adherence, and preventive screenings rather than solely relying on age, location, or income.
For example, in a colorectal cancer screening campaign, Engagys demonstrated that segmentation based on previous preventive actions rather than general demographics yielded higher engagement. In this case, messages tailored for those who frequently use preventive services could be distinct from those directed at members who are disengaged or lack a primary care provider. By segmenting based on actual behavior, health plans can offer interventions that are both personalized and predictive, meeting members where they are in their healthcare journey.
AI for Real-Time Personalization: From Broad Segments to “N of 1”
AI enables segmentation down to an N of 1, or individual level, by analyzing vast data points across multiple sources, including audio and video data, call center transcripts, and even social media. Traditional segmentation often grouped members into broad categories, which can be too general to drive meaningful engagement. With AI, health plans gain insights into both the actions a member might take and the barriers that may prevent them, allowing for more impactful, personalized interactions.
We’ve seen the power of AI-driven personalization when working with a health plan to refine their approach to encouraging annual wellness visits. By identifying members who faced transportation issues, Engagys helped the plan tailor messages that emphasized transportation support options. This targeted communication led to a 15–20% increase in wellness visits among members using the transportation benefit. Such precision in addressing specific needs makes AI-driven segmentation a game-changer in fostering meaningful member engagement.
Implementing AI-Driven Segmentation: Best Practices and Pitfalls
As AI reshapes segmentation, health plans must adhere to best practices to avoid potential pitfalls. We suggest starting small with specific actions. Instead of trying to address all engagement needs simultaneously, health plans should begin with one goal, such as improving mammogram rates or flu vaccinations. This allows for more manageable implementation and clearer measurement of outcomes. For instance, breaking down member actions into smaller segments based on behavior—like flu shot reminders for members actively receiving routine care—proves more effective than a one-size-fits-all approach.
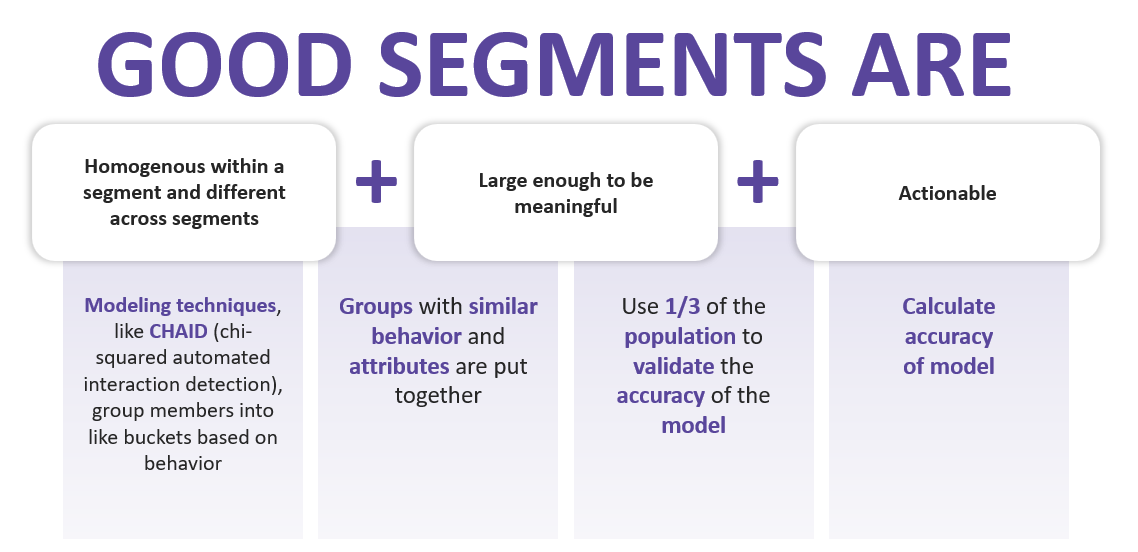
Another key takeaway is the need for AI segmentation to be dynamic and validated through testing. Don’t assume that AI has created the perfect segments through its ability to detect patterns. Taking time to validate and even train how it interprets patterns is key to success. Additionally, one important note is that when segments are done well, they don’t change except in the face of big environmental impacts, such as those seen during the COVID-19 pandemic. Importantly, even though segments done well don’t need frequent refreshing, where consumers fall within those segments is dynamic and can change quickly with life stage, a new diagnosis, and more. AI can facilitate this adaptability, but health plans should regularly test their positioning to consumers within segments through A/B testing frameworks to ensure they remain relevant and optimized. Experimentation allows health plans to learn from each iteration, fine-tuning communications based on what resonates best with members.
Lastly, it’s crucial for health plans to address the challenges that come with AI-driven segmentation. Engagys found that some AI tools are better suited for healthcare than others; using non-verticalized AI tools may increase member abrasion due to overly generic or irrelevant messaging. Therefore, investing in healthcare-specific AI solutions and governance to prevent interaction collisions can help health plans use AI effectively and avoid unintended consequences.
The Future of AI-Powered Member-Centric Engagement
AI-driven segmentation represents a new era for health plan engagement, where the focus shifts to member-centric interactions that are informed by individual behaviors and contextual data. For health plans, this evolution means greater ability to influence member behaviors, from preventive screenings to medication adherence, through tailored messaging that resonates on a personal level. However, success with AI-driven segmentation requires careful planning and training, continuous validation, and a commitment to leveraging the right data to guide decision-making.
Health plans are still in the early stages of fully realizing AI's potential. Yet, as more plans implement AI for segmentation, the benefits are clear: higher engagement rates, improved health outcomes, and a stronger connection between members and their health plans. By embracing the insights AI provides, health plans can finally deliver on the promise of a personalized healthcare experience that members not only value but also trust.


